Pertussis Outbreak at Upper Columbia Academy in Spangle, WA
Posted Nov. 14, 2018. Past health advisories and alerts are archived for historical purposes and are not maintained or updated.
Current Situation
At least 25 high school students and staff members at Upper Columbia Academy (UCA) in Spangle, WA have compatible illness with B. pertussis, including two lab-confirmed cases. The onset of the outbreak was mid-September; however, the first lab confirmed case was identified late last week. UCA is a private Seventh-day Adventist boarding school for approximately 200 high school students from the Northwest and all over the country. A small elementary school for local students and a church attended by students, staff, and local families are also present on the UCA campus.
Actions Requested
- Be aware of the current outbreak affecting students and staff at Upper Columbia Academy.
- Provide treatment to symptomatic individuals connected to UCA and post-exposure prophylaxis to exposed individuals as recommended in the guidelines below.
- Test Spokane County residents for pertussis with PCR if they have compatible illness.
Post-exposure Prophylaxis Guidelines
Given the large numbers of ill students and staff, SRHD is considering the following groups to be exposed:
- All high school students and high school staff at UCA
- All family members and close contacts (significant others, close friends) of symptomatic students and staff
- Church members who sat next to a coughing student/staff member or had another close contact* exposure to a symptomatic individual while coughing
- Visitors who had close contact* with a symptomatic student/staff member while coughing
*Examples of close contact include direct face-to-face contact; an obvious exposure that involves direct contact with respiratory, oral, or nasal secretions from a case-patient (a cough/sneeze in the face, kissing, sharing eating utensils, etc.), and close proximity for a prolonged period of time (risk of exposure increases with longer duration and closer proximity of contact). Close contact does NOT include activities such as walking by a person or briefly sitting across a waiting room or office from someone.
CDC and SRHD support targeting post-exposure prophylaxis (PEP) antibiotic use for people at high risk of developing severe pertussis, as well as people who will have close contact with others at high risk of developing severe disease. Due to the close-knit, family community of UCA, SRHD supports the use of PEP in exposed students and families at the campus within 21 days of exposure as follows:
- All household contacts of a pertussis case (known positive or epidemiologically linked with a compatible illness) to include family members that spent time with the case while contagious and/or roommates, significant others, close friends, etc.
- High-risk people exposed to a pertussis case (known positive or epidemiologically linked with a compatible illness). High-risk people are those who personally are at high risk of developing severe illness, or those who will have close contact with people at high risk of severe illness. These include:
- Infants, and women in their third trimester of pregnancy
- All people with pre-existing health conditions that may be exacerbated by a pertussis infection (e.g., immunocompromised people, those with moderate to severe asthma, etc.)
- People who themselves have close contact with either infants under 12 months, pregnant women or individuals with pre-existing conditions
- All people in high-risk settings that include infants under 12 months or women in their third trimester of pregnancy (neonatal intensive care units, childcare settings, etc.
No illnesses have been confirmed in the elementary school at this time. However, there is some interaction between elementary and high school students at UCA and exposure assessments should be done individually.
If after assessing exposure it is not clear whether an exposure occurred, it is appropriate to encourage the exposed person to watch for signs and symptoms of pertussis for 21 days following their last exposure to a symptomatic person. These exposed persons should be instructed to seek healthcare immediately at the first sign of compatible illness
About Pertussis
Pertussis, more commonly known as whooping cough, is a contagious, respiratory disease caused by the bacterium Bordetella pertussis. The illness is typically characterized by a prolonged paroxysmal cough that is often accompanied by an inspiratory whoop. Disease presentation can vary with age and history of previous exposure or vaccination. Young infants may present to a clinic or hospital with apnea and no other disease symptoms. Adolescents and adults with some immunity may exhibit only mild symptoms or have the typical prolonged paroxysmal cough. In all persons, cough can continue for months. Infants are at greatest risk for pertussis-related complications and mortality. The Centers for Disease Control & Prevention (CDC) maintains a thorough overview of the clinical features of each stage of illness.
Early diagnosis and treatment of pertussis might limit its spread to other susceptible people. When pertussis is strongly suspected, attempts to identify and provide prophylaxis to household and other close contacts at high risk should proceed without waiting for laboratory confirmation.
Testing
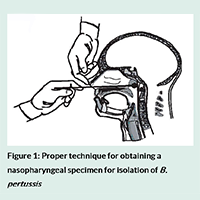
Determining who has pertussis and who does not can be difficult, particularly during the catarrhal phase when symptoms can be indistinguishable from those of minor respiratory tract infections (coryza, low-grade fever, mild cough). Whenever possible, a nasopharyngeal swab should be obtained from all persons with suspected pertussis for PCR testing. A properly obtained nasopharyngeal swab or aspirate is essential for diagnosis. CDC has produced training videos on proper specimen collection.
Antimicrobial Treatment & Prophylaxis
Antimicrobial treatment does not generally lessen the severity of disease unless it is begun in the catarrhal phase, prior to paroxysmal coughing. However, early treatment reduces transmission and is essential for disease control. Persons with pertussis are infectious from the beginning of the catarrhal stage through the third week after the onset of paroxysms or until five days after the start of effective antimicrobial treatment.
The recommended antimicrobial agents and doses are the same for both treatment and chemoprophylaxis. Three macrolides are recommended by CDC for treatment of pertussis. Azithromycin is most popular because it is given in a short, simple regimen of one dose each day for five days. Full treatment guidelines are available from the CDC.
Vaccination
Vaccination is the most effective way to prevent pertussis. Babies and children should get five doses of DTaP for maximum protection. A booster dose of Tdap is given to preteens at 11 or 12 years old. Teens or adults who didn’t get Tdap as a preteen should get one dose. Pregnant women should also receive a dose of Tdap during each pregnancy in the third trimester.
Pertussis vaccines are effective, but not perfect. They typically offer good levels of protection within the first two years after getting the vaccine, but then protection wanes over time. In general, DTaP vaccines are 80% to 90% effective. Among children who get all five doses of DTaP on schedule, effectiveness is very high within the year following the 5th dose – at least nine out of ten kids are fully protected. There is a modest decrease in effectiveness in each following year. About seven out of ten kids are fully protected five years after getting their last dose of DTaP and the other three out of ten kids are partially protected – protecting against serious disease.
CDC’s current estimate is that in the first year after getting vaccinated with Tdap, it protects about seven out of ten people who receive it. There is a decrease in effectiveness in each following year. About three or four out of ten people are fully protected four years after getting Tdap.
