Update: Novel Coronavirus (COVID-19) in China
Posted Feb. 13, 2020. Past health advisories and alerts are archived for historical purposes and are not maintained or updated.
Public health agencies continue to monitor the outbreak of novel coronavirus (name changed on 2/11/20 to COVID-19 from 2019-nCoV, per the World Health Organization) that originated in Wuhan City, Hubei Province, China in late December. To date, almost 99% of the more than 45,000 confirmed cases globally have occurred in China; nearly 74% of these occurring in Hubei Province. A map of eastern Asia and a flow chart to help identify suspect COVID-19 cases are attached to this advisory.
Public health continues to recommend healthcare providers consider COVID-19 in a patient who has traveled from China presenting with fever, cough or shortness of breath. Do not consider COVID-19 in patients with travel outside of China unless the patient is a close contact of a known COVID-19 case. We recognize fear and uncertainty have resulted in significant concern among many patients and healthcare providers, and some patients may demand testing even without risk of infection. Testing is restricted to strict case definition criteria that include both travel to China (or contact to a confirmed case) and compatible symptoms. Public health will not authorize testing for asymptomatic individuals.
As of February 2, the United States expanded airport screening to all incoming travelers from China.
- All travelers from Hubei Province are considered high risk and are placed under mandatory federal quarantine for 14 days from the day they left China.
- All travelers from mainland China are considered medium risk. They will be contacted by local public health and asked to stay home and away from others for 14 days from the day they left China while self-monitoring for symptoms. Travelers are instructed to call public health if they become symptomatic so a medical evaluation can be coordinated safely.
For all patients
- Obtain a detailed travel history for patients being evaluated with fever and symptoms of acute lower respiratory illness (cough and/or shortness of breath).
- Use the attached COVID-19 Evaluation Tool for Healthcare Providers to assist in screening for possible COVID-19 infection
When to suspect COVID-19
- COVID-19 should be suspected in patients who present with:
- fever AND symptoms of lower respiratory illness (e.g., cough, difficulty breathing) AND in the 14 days before symptom onset:
- have a history of travel from China --OR--
- had close contact with a person who is under investigation for COVID-19 while that person was ill.
- fever OR symptoms of lower respiratory illness (e.g., cough, difficulty breathing) AND in the 14 days before symptom onset had close contact with an ill lab-confirmed COVID-19 patient.
- fever AND symptoms of lower respiratory illness (e.g., cough, difficulty breathing) AND in the 14 days before symptom onset:
- While there have been concerns voiced in the media about asymptomatic infections, public health will not approve specimens for testing from asymptomatic individuals with travel from China or for symptomatic individuals who have had contact with asymptomatic people who had travel from China.
If above criteria are met to suspect COVID-19
- Ask patients with suspected COVID-19 infection to wear a surgical mask as soon as they are identified and evaluate them in a private room with the door closed, ideally an airborne infection isolation room if available.
- All healthcare personnel entering the room should use standard precautions, contact precautions, airborne precautions, and use eye protection (e.g., gown, gloves, N95 mask or PAPR, and face shield or goggles).
- Immediately notify both infection control personnel at your healthcare facility and Spokane Regional Health District at 509-869-3133 in the event of a suspected case of COVID-19.
- Collect an upper respiratory specimen (NP or OP swab) and store in viral transport medium. Specimens should be refrigerated and shipped cold. Public health will provide guidance and facilitation regarding specimen collection, storage, and shipping.
- Concurrent local commercial testing of a second upper respiratory specimen should occur with a respiratory pathogen panel to rule out other infectious causes, including but not limited to influenza.
- Outpatient settings should consider transfer of a patient presenting with possible COVID-19 infection to an emergency department where PPE and an airborne infection isolation room may be more readily available to help aid in the safe collection of specimens and minimize risk to healthcare workers.
DOH and CDC have compiled additional guidance for healthcare providers, which is available on their website (this is a rapidly evolving situation and you should continue to check the Washington DOH website for updates to these documents:
- Novel Coronavirus (COVID-19) Evaluation Tool for Healthcare Providers
- Novel Coronavirus Fact Sheet for Patients
- Healthcare Infection Prevention Guidance for COVID-19
- Healthcare Professional Preparedness Checklist for Transport and Arrival of Patients Potentially Infected with COVID-19
- Hospital Preparedness Checklist for Suspected or Confirmed COVID-19 Patients
- COVID-19 Specimen Collection and Submission Instructions
- Lab Biosafety Guidelines
Additional Resources
- COVID-19 Global Cases, GIS Mapping, Johns Hopkins Center for Systems Science and Engineering
- Information for Healthcare Professionals: https://www.cdc.gov/coronavirus/COVID-19/guidance-hcp.html
- Interim Guidance for Preventing Transmission in Homes and Communities: https://www.cdc.gov/coronavirus/COVID-19/guidance-prevent-spread.html
- Guidance for Travelers: https://wwwnc.cdc.gov/travel/notices/watch/novel-coronavirus-china
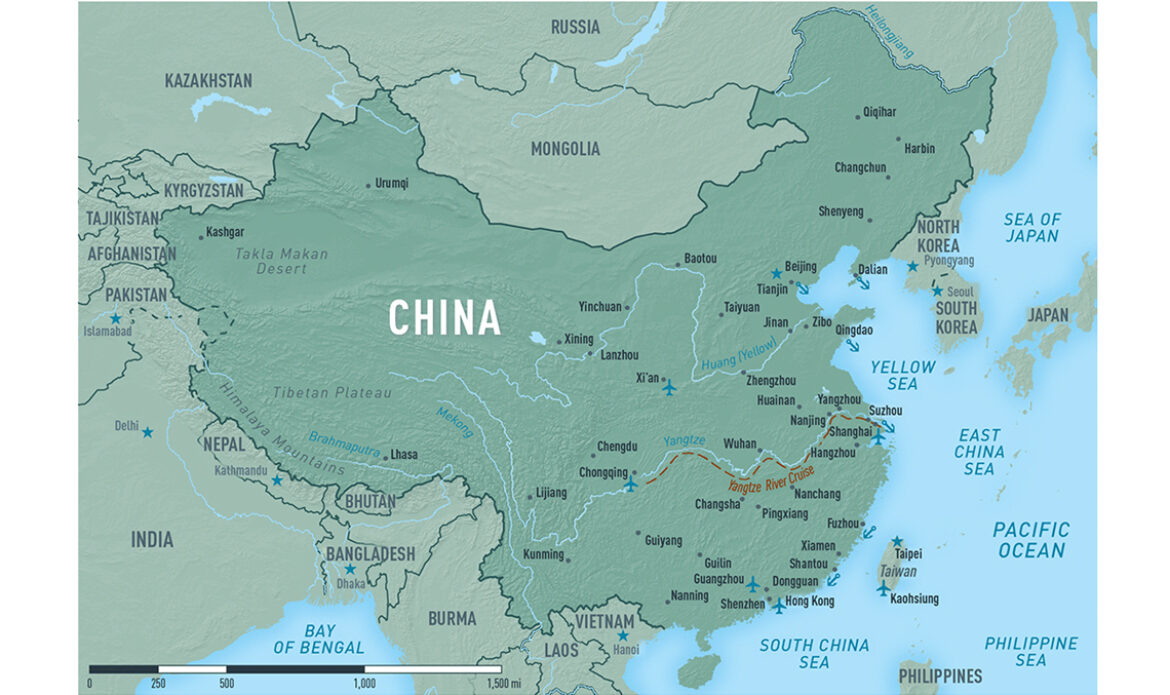
Map courtesy CDC