Coronavirus Mutations and Variants: What Does It Mean?
By: Francisco R. Velázquez, M.D., S.M.
Organisms in general, be it humans, plants, insects, bacteria, or viruses, undergo genetic mutations which can be beneficial or detrimental. Although viruses are not technically alive, these also mutate and evolve as they infect a host’s cell, replicate and move on to another cell or a new host. The process by which a virus spreads is what we call transmission. There are differences in the rates of mutations amongst different types of viruses. As an example, the SARS-CoV-2 coronavirus which causes the clinical entity we know as COVID-19 mutates approximately every 11-15 days. That is about half of the rate of influenza (flu) and about a quarter of the HIV rates. Mutations generate variability within a population, which allows natural selection to amplify traits that are beneficial, in this case, to the viral particle, as viruses are not considered organisms per-se.
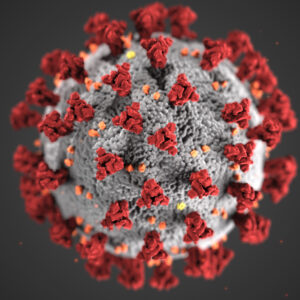
We know the coronavirus currently has 12,700 identified mutations, 12 main types of the virus (identified as 19 A, the original type, through 20 J), five strains and almost 4000 variants. The strains are known as L, the original strain, which mutated into the S strain followed by V and G (further mutating into GR, GH and GV, and several infrequent mutations collectively grouped together as O). The G strains are now the dominant strain around the world. SARS-CoV-2 variants with spike (S)-protein D614G mutations have become the most common variant. It is so named because one amino acid is changed from a D (aspartate) to a G (glycine) at position number 614 of the viral spike proteins. The spike protein mediates the binding to the target receptors and the fusion to the human cell membrane. The S protein extends from the viral membrane giving the virus surface a crown-like appearance, for which the virus is named; corona is crown in Latin. Most of the variants of concern contain mutations in the receptor-binding domain (RBD). It seems these mutations are responsible for increased viral infectivity, virulence, and immune evasion potency. It is known that the RBD is involved in viral recognition and cell receptor binding and interaction, thus any structural changes seem to be directly related to viral transmissibility and virulence. It has also been identified in numerous studies that antibodies developed against the RBD have been found to have maximum potency against the SARS-CoV-2.
It all starts in the coronavirus RNA genome, which is composed of 30,000 nucleotides, the basic structural unit of nucleic acids. The best way to think about it is as an alphabet of 30,000 letters that spell the sequences for 29 genes. The virus itself is a coil of genetic material in a protein shell with an outer envelope most of the time. The virus binds to a human target cell receptor, injects its genetic material, and takes over the cell, turning into a virus replicating factory. As it replicates, mutations can take place and either help or compromise the virus. Many of the identified mutations are inconsequential as these do not change the biology of the virus. Mutations are passed down through lineage, best described as a branch in the family tree. A group of coronaviruses that have the same inherited set of very distinctive mutations is called a variant. The lineage becomes known as a strain, and in this specific example, COVID-19 is caused by a coronavirus strain known as SARS-CoV-2. Through the course of the pandemic, we have identified several variants globally, five of which are of concern as the strains are associated with higher transmission rates that may impact the effectiveness of vaccine and therapy, and it seems increased mortality may be associated with at least one variant. More recently there have been several variants identified in the United States that share some mutations with the more aggressive variants initially identified in other countries.
The first step in understanding the variants and the impact these have in infection, reinfection and possible effects on vaccines and treatments is knowing the mutations. Although there are thousands of mutations for the most part, thus far, seven of those are the most critical to know.
D614G Spike Mutation
The D614G Spike mutation was the first mutation of concern identified in China early in the pandemic. This mutation quickly spread around the world allowing the mutated viruses to rapidly replace strains without the mutation. Although it seemed to increase the infectiousness, it was not associated with more severe disease or reduced vaccine effectiveness.
A222V Mutation
The first variant-associated mutation seen in Europe is known as A222V, identified in the B.1.177 (20A.EU1) variant that originated in Spain and dominated the European landscape for months. We do not hear much about it, because it has not been associated with increased transmission.
N501Y Spike Mutation
More of concern are the next five mutations identified. First is the N501Y Spike mutation which has been identified in at least three variants of concern. Found at the tip of the Spike protein, this mutation seems to cause a tighter thus more effective fit to the human cell receptors.
E484K Spike Mutation
The E484K Spike mutation is of significant concern as it has been identified not only in three of the global variants, but also in the newly described American variants. It has been observed in vitro that this mutation alters the shape of the proteins in the viral spike which can potentially mask the antigenic portion from antibodies. There has been much speculation as whether this mutation may impact the effectiveness of monoclonal antibody treatments and cause reinfection in some patients.
L452R Mutation
The next mutation, although infrequent in the United States, has been associated with many cases in California. L452R has triggered the emergence of numerous global variants and is present in the two recently identified California variants which also carry other mutations. The L452R mutation might enhance the interaction between virus and host cell, which in turn may significantly increase viral transmission and virulence. It may also reduce the virus-neutralizing ability of antibodies specifically targeting the spike RBD.
K417N/T Mutation
The sixth is the K417N/T mutation located on the tip of the spike protein, an area important to the antibody recognition process. In some experiments the K417N/T mutation has been associated with decreased antibody recognition and possible resistance to some antibodies. The possibility of a more effective virus/cell binding process has also been described.
Q677 Mutation
More recently the Q677 mutation has been described in at least seven lineages initially identified in Louisiana and New Mexico. It’s now in seven states, mainly in the south central and southeast United States. This mutation is four amino acids away from the S1/S2 cleavage site, an area where other mutations have been identified in the more infectious strains. It is unclear currently whether this mutation increases transmission rates.
B.1.1.7 Variant
The centers for Disease Control have defined three different levels of threat associated with variants. These are variants of interest (B.1.526, B.1.525 and P.2), variants of concern (B.1.1.7, P.1, B.1.351, B.1.427 and B.1.429), and variants of high consequence. In the U.S. we have identified the first two categories only. For the variants of concern there is evidence of increased transmissibility, more severe disease and reduced therapeutic effectiveness. Currently, globally-identified variants have been detected in multiple states. First identified in the United Kingdom is the variant known as B.1.1.7, now present in at least 90 countries and 51 states including Washington. This variant accumulated a high number of mutations including several in the spike protein. Of the 17 identified, the most notable is the N501Y mutation which has been found to help the virus form a tighter attachment to the ACE2 receptors. This variant is approximately 50% more infectious than the wild type of virus and is estimated to be doubling in the U.S. every 10 days.
B.1.351 Variant
Just as the B.1.1.7 variant was being identified, another variant with the same type of N501Y mutation was identified in South Africa. This variant is known as B.1.351 and contains additional mutations such as the K417N, and of more concern the E484K mutation. The latter has been identified in 48 countries and 30 states including Washington. In vitro studies have suggested a potential for a blunted immune response, and a small impact on vaccine efficacy.
P.1 Variant
A variant that originated in Brazil was first reported in Japan, as it was identified on four people screened upon arrival at an airport outside of Tokyo. It is postulated that the travelers acquired the variant known as P.1 while in Brazil where the lineage is traced back to the city of Manaus, the largest city on the Amazon region. This variant has 17 unique mutations in the spike protein that include the N501Y, E484K and K417N previously discussed. It has been identified in at least 25 countries and 22 states, including Washington. Of particular concern is the anecdotal reports of reinfection in people who had recovered from disease.
CAL.20C – B.1.427 and B.1.429
Several other variants have been identified in the U.S. over the past several months. One of these variants with the L452R mutation was identified in California and is considered a variant of concern. The variant designated as CAL.20C has two forms: the B.1.427 and B.1.429. It is believed to cause a stronger attachment that may prevent neutralizing antibodies from interfering with the attachment process. Additional work is needed in determining the impact this has in transmissibility, and disease severity.
B.1.526 and B.1.525
The B.1.526 and B.1.525 Variants identified in New York and traced back to Washington Heights, a Manhattan neighborhood, the B.1.526 variant has two types: one with the E484K spike mutation which may blunt the antibody response and another with the S477N mutation that may increase the effectiveness of the attachment process. The E484K mutation is also present in the Brazilian and South African variants. These, in addition to the P.2 identified in Brazil, are currently classified as variants of interest.
Novel Midwest Variants
In the Midwest, specifically in Columbus, Ohio, two novel SARS-CoV-2 clade 20G variants have been identified. The predominant variant has several mutations, including the Q677H and has been identified in several states in the upper Midwest. It is referred to as the “Midwest” variant. Subsequently, a second variant with the S N501Y mutation, which is a marker of the B.1.1.7, but lacking all other mutations associated with that strain has been identified. This mutation has also been associated with the South African variant. It will be important to further determine what impact these variants will have in the overall pandemic pattern.
It is important to remember that what most of these variants have in common is a more effective transmission pattern, which has been associated with a surge in infections in various areas of the world. In addition, some data suggest that increased morbidity and perhaps mortality can be associated with some of the variants. The impact on treatment and vaccines is still being determined, although preliminary data points to minimal impact on vaccine efficacy. Moreover, vaccine manufacturers have significant capabilities in the reformulation of vaccines.
We also know the transmission mode is the same as with the wild-type (unchanged) coronavirus, thus preventing infection should follow a similar public health guidance: facial coverings, social distancing, avoiding gatherings, and practicing appropriate hygiene and sanitation. These simple rules along with increased immunization and appropriate levels of testing continue to be the key pillars in our management of the pandemic.
