Sensitivity, Specificity, Positive Predictive Value… Oh My!
With the definitions of sensitivity and specificity often erroneously used interchangeably, it is easy to forget their true meaning. It is important to take into account a test’s sensitivity and specificity, as well as positive and negative predictive values, when making testing decisions and subsequent diagnoses.
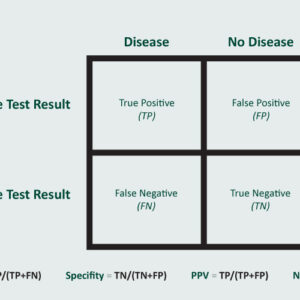
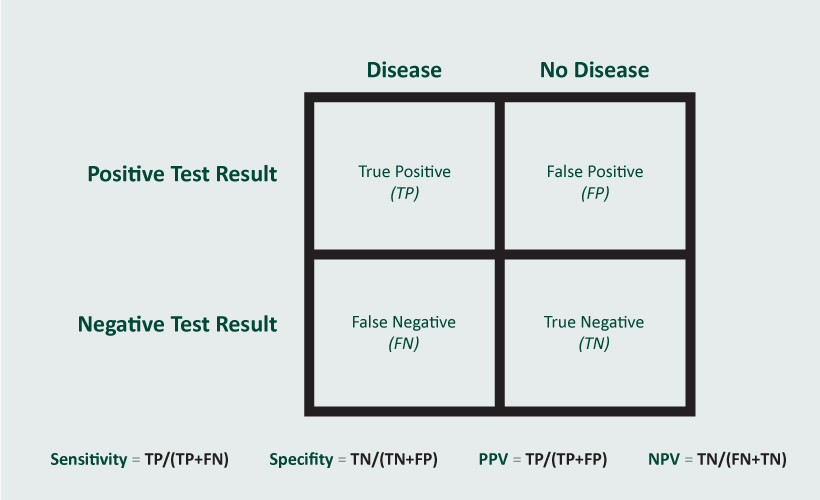
Sensitivity refers to the true positive rate, specifically: (true positives)/(true positive + false negative). A test’s sensitivity provides you with the percentage chance (or likelihood) it will correctly identify a person who has the disease. In other words, if the test is highly sensitive and the test result is negative, you can be nearly certain the person you’re testing does not have the disease. If a test has a 90% sensitivity, it will identify 90% of persons with the disease.
Specificity refers to the true negative rate, specifically: (true negatives)/(true negative + false positive). A test’s specificity tells you the percentage chance it will correctly identify a person who does not have the disease. In other words, if the test is highly specific and the test is positive, you can be nearly certain that the person you’re testing has the disease. If a test is 90% specific, it will identify 90% of those persons who do not have the disease.
For screening, a clinician will want a very sensitive test. While for confirmation, a clinician will want a very specific test.
An example of a test that is both highly sensitive and specific is the B. pertussis PCR (polymerase chain reaction), with sensitivity and specificity at or near 100%, meaning all or almost all positives will be true positives, and all or almost all negatives will be true negatives (allowing for some variation with collection technique, of course).
Conversely, the mumps RT-PCR and viral culture are notoriously unreliable in previously vaccinated persons, resulting in poor sensitivity. Vaccinated individuals may shed virus for a shorter period and might shed smaller amounts of virus, thereby making detection in RT-PCR dependent on timing of collection and the quality of the sample. For serology, the ability to detect IgM is highest in unvaccinated persons (80-100%) and the lowest in two-dose vaccine recipients (13-14%).
Positive predictive value (PPV) and negative predictive value (NPV) are equally important but represent a different perspective. PPV refers to the probability that a person with a positive screening test truly has the disease, while NPV refers to the probability that a person with a negative screening test truly does not have the disease. The PPV will tell you how worried someone with a positive test should be and the NPV should tell us how reassured someone with a negative test should be. These values are affected by the prevalence of disease in a population.
At low prevalence, the PPV will decrease and the proportion of false-positive test results will increase. A Spokane-specific example of this is Lyme disease testing. We are a low prevalence area and false-positive tests are common, marking a low PPV. Inversely, chlamydia screening in a high prevalence population (such as women under the age of 25) will have a higher PPV and a lower proportion of false-positive results.
