Lyme Disease Testing: CDC Recommends a Two-Step Process
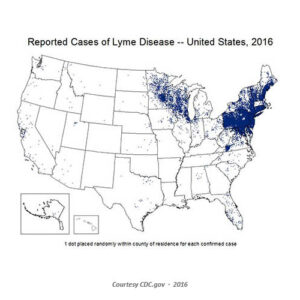
Lyme disease is rarely acquired in Washington state, and when it is acquired in-state, it is almost always west of the Cascades. If a healthcare provider suspects a person has been exposed to Lyme disease in an endemic area, such as the upper Midwest region, Eastern US, or the West Coast, or to an animal from these regions, the CDC currently recommends a two-tiered process for testing. Both can be done using the same blood sample.
The first uses an enzyme immunoassay (EIA), or rarely an immunofluorescence assay (IFA), to measure the overall immune response (IgG and IgM). First-tier testing has a high sensitivity that increases the likelihood of identifying a true positive case. A positive or equivocal result is followed by a highly specific Western immunoblot test as the second-tier to confirm the diagnosis and rule out false positives. A negative first-tier result suggests no further testing is required. Second-tier testing also measures the immune response to infection, with the type based upon the duration of illness. As antibody levels are low during the “window period” of the immune response, IgM is the first immunoglobulin to develop, but is useful only during the first 30 days of illness. Reflex Western immunoblot testing for both IgM and IgG should be ordered for symptoms less than 30 days. Most individuals should will have adequate IgG antibody levels for detection 30 days of presumed infection. Therefore, only IgG Western immunoblot testing should be ordered, as testing for IgM increasing the likelihood of false positive results. A positive Western immunoblot IgG test result is confirmatory for disease.
The two-tiers are designed to be concurrently; the CDC does not recommend skipping the first test and proceeding directly to the Western immunoblot. Doing so will increase the frequency of false positive results and may lead to misdiagnosis and improper treatment. Results are considered positive only if both the EIA and the immunoblot tests are positive. It should be noted the sensitivity of 2-tiered testing is low (30%–40%) during early infection (window period) as the antibody response is developing, but increases for disseminated disease; the specificity is high (>95%) during all stages of disease. It should also be noted false positive first-tier test results may occur because of other diseases, such as tick-borne relapsing fever, syphilis, anaplasmosis, leptospirosis, some autoimmune disorders (e.g., lupus), bacterial endocarditis, and/or infection with H. pylori, Epstein Barr virus, or Treponema denticola.
