Infection Control in Outpatient Settings: Beyond OSHA
Changes in healthcare have caused a shift of care to outpatient settings and specialized services. This has not lessened the complex needs of some patients, however. These individuals rely on frequent and intensive use of outpatient care to maintain and improve their health. They are vulnerable to infection from the increased frequency of invasive procedures, use of antibiotics, immunocompromise, age, and multiple co-morbidities, such as diabetes, advanced renal disease, and obesity, to name a few.
One of the most profound lessons of the 2013-16 Ebola outbreak is that of controlling the transmission of infection. Given the developed world has the knowledge, technology, and resources available to prevent most transmissions, dissemination of this knowledge and implementation of appropriate practices are essential. Unfortunately, nosocomial, or healthcare-associated infections (HAIs), remain a significant problem and are the focus of national and international efforts.
Infection prevention and control (IPC) in the outpatient setting involves every employee – front desk staff, volunteers, custodians and healthcare professionals. IPC also includes every patient and visitor – anyone with the potential for indirect, e.g., contaminated equipment, surfaces, or air, or direct contact with ill persons and/or to their body fluids. In turn, a robust IPC program protects everyone, including the healthcare providers and patients.
Infection prevention begins at the facility door, with signage encouraging visitors to cover their coughs/sneezes, and providing masks, tissues and hand hygiene supplies. Initial triage of patients should include obtaining a history of multi-drug resistant organisms, occupation, and recent travel history. Travel screening should include any out-of-area travel in the past 2-3 weeks, which can alert for possible exposure to infectious agents (for example, there have been ongoing outbreaks of Hepatitis A in communities across the US, as well as outbreaks of measles, both in the US and abroad). Vaccination history is also an important component part of patient intake. (For information on how to access the Washington Immunization Information System (IIS), contact Kari Lidbeck at 509.324.1649 or KLidbeck@srhd.org).
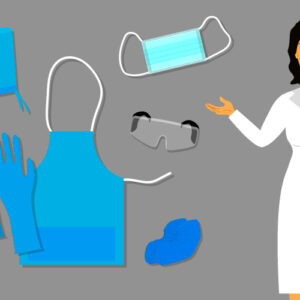
Evidence-based policies and procedures, which consider the types of services conducted and the population served, further direct IPC activities. Components of a good IPC program include: designated personnel responsible for infection prevention activities who have had formal training and are given financial support/time to do the work; competency-based training on hand hygiene, personal protective equipment (PPE), injection safety, point-of-care testing, environmental cleaning, and device reprocessing; adequate supplies of devices appropriate to the tasks performed, which can be properly cleaned and disinfected, as well as appropriated machinery and supplies to perform those processes. HCP safety can also be bolstered by policies that require/promote vaccination of staff and patients, and sick leave policies that encourage staff to stay home when ill. Protecting staff and patients from infection greatly contributes to protecting public health. Through a grant funded by CDC, the Spokane Regional Health District (SRHD) employs a certified Infection Preventionist who can assist facilities with assessing their IPC, using the Infection Control Assessment and Response (ICAR) tool. The ICAR is voluntary, free, and non-regulatory. If organizations, clinics or facilities are interested in having an assessment performed, contact Dorothy MacEachern at 509.324.1569 or dmaceachern@srhd.org. Dorothy will travel to facilities in eastern and central Washington or in northern Idaho.
