The Return of Syphilis
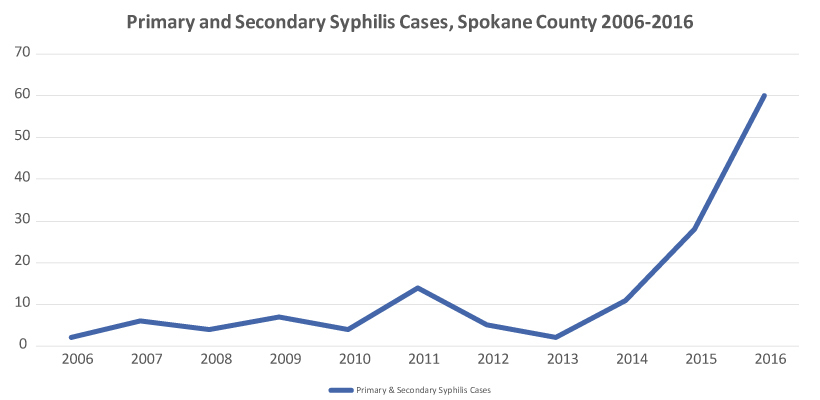
Syphilis is back. Cases of infectious syphilis continue to increase in Spokane County, a concerning trend first noted in 2015 when 28 cases of primary and secondary (P&S) cases were reported, a 154% increase over the previous year. In 2016, P&S cases increased still with 60 cases reported; the trend continues this year.
Additionally, with increased infection in the Spokane community, the epidemiology shifted. Prior to 2015, most infectious cases of syphilis were diagnosed in men who have sex with men (MSM). Presently, MSM account for only about 20% of cases diagnosed; nearly half of all cases are reported in women, some of whom were diagnosed in pregnancy. Subsequently, there has been one syphilitic stillbirth and two infants diagnosed with congenital syphilis in 2017—firsts for Spokane County. To help slow the spread of syphilis and reduce the likelihood of additional congenital cases, providers are asked to take the following actions:
- Test all patients who request STD testing for syphilis, particularly those presenting with symptoms of HSV
Screen for syphilis with a treponemal antibody EIA that will reflex to additional testing, if needed; if you use PAML, use order code TREP. If the treponemal EIA test is positive, it will reflex to an RPR titer. If the RPR is negative, it will reflex to a second treponemal test, the TPPA, for confirmation of syphilis infection. If two of the three tests are reactive, the patient has syphilis or had syphilis. Lab results alone cannot always differentiate between old and new infection. STD Prevention staff at SRHD can access your patient’s syphilis test and treatment history, and can assist with interpreting test results, determining staging, and/or treatment recommendations. - Look for symptoms of syphilis; symptoms vary based on stage of infection
Primary: Every person infected with syphilis will have a primary lesion or chancre located at the point of inoculation, typically in or around the mouth, genitals, or rectum. The highly-infectious chancre is easily mistaken as HSV lesions. Some patients may attribute their sore to a cut from shaving, ingrown hair, or friction burn. Lymphadenopathy may be present.
Secondary: Infectious symptoms of secondary or systemic syphilis include mucous patches in the mouth and/or condyloma lata (moist HPV-like growths) in or around the genitals, including the inner thighs. Other symptoms include a rash on the trunk, a palmar/plantar rash, or patchy hair loss. Many patients also experience flu-like symptoms and lymphadenopathy.
Latent: Patients with a positive lab, no symptoms of active infection, and no prior treatment history are considered latent syphilis cases. Patients can be staged as early latent (infected less than 12 months) or late latent (infected more than 12 months). STD Prevention staff at SRHD can assist in determining staging; when in doubt, plan to treat these patients as late latent cases.
Neurosyphilis: Central nervous system involvement can occur during any stage; screen all patients diagnosed with syphilis for changes in hearing, vision, or cognitive function. If present, a lumbar puncture and treatment with IV antibiotics may be indicated. - Treat patients appropriately based on their stage of infection
For a symptomatic patient, a one-time injection of 2.4 million units of benzathine penicillin G (Bicillin-LA) is adequate. For patients with late syphilis, three doses of Bicillin-LA given a week apart may be needed. If you have a lab-confirmed or suspected case of syphilis, SRHD has a stock of Bicillin, provided by Washington Department of Health, that we can deliver to your office at no cost to you or the patient. Call 509-324-1609 for assistance.
For patients with a penicillin allergy, doxycycline is currently the only CDC-approved alternate treatment. For pregnant women with a penicillin allergy, desensitization is required so they can receive Bicillin. -
Screen for Syphilis in Pregnancy
Screening for syphilis at the initial prenatal visit is essential for reducing the likelihood of congenital syphilis cases, but it may not be enough. In both cases of congenital syphilis reported this year, the mothers had a negative syphilis test at their initial prenatal visit. For high-risk women (i.e., multiple partners, new partner during pregnancy, STD diagnosis in pregnancy, substance use in pregnancy), re-screen your patient during the third trimester and again at delivery. For women who are found to have syphilis in pregnancy, immediate treatment, partner treatment, and close follow-up are important to prevent stillbirth or the baby born with congenital syphilis.
Call Julie Zink at 509.324.1609 or Kirsten Duncan at 509.324.1635 for assistance.
