Focus on Mumps
Spokane Mumps Outbreak 2016-2017: In Numbers
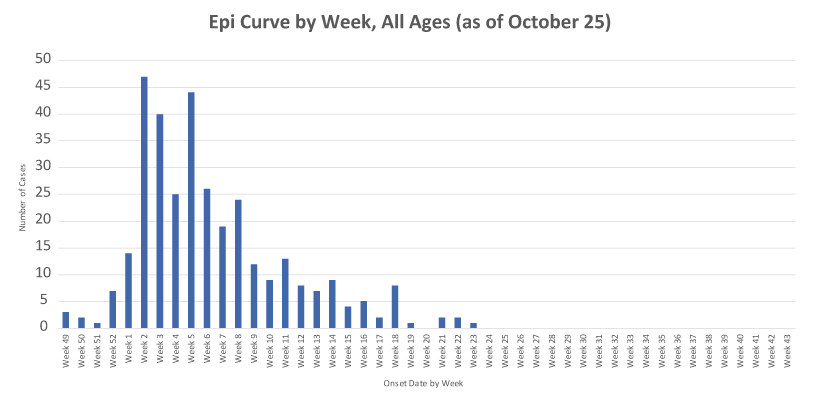
Within the course of a few weeks, a handful of isolated mumps cases in King County in November 2016 exploded into a statewide mumps outbreak that continued into early January 2017. Spokane’s first mumps case was reported mid-December 2016, with cases peaking in January and early February. Spokane Regional Health District (SRHD) Epidemiology staff theorized the holidays contributed to the explosion of cases across the state, as families traveled and gathered together while celebrating in close spaces with shared foods and beverages.
Washington State Department of Health (DOH), Tacoma Pierce County Health Department, Panhandle Health District, and Northeast Tri-County Health District all stepped in to assist with case interviewing for Spokane County. Washington Poison Center handled the extraordinary volume of phone calls with questions from the public coming in to SRHD. This outbreak was extremely taxing on local public schools and families, the medical community, and other public health partners. The Spokane outbreak was declared over this June and was the largest in recent memory.
- Reported confirmed/probable cases: 333
- Reported suspect cases: 97
- Total possible cases investigated: 682
- SRHD costs: $169,639.20
- Adult MMR doses given or documentation provided: 7,539 between Oct. 1, 2016 (baseline) and Aug. 11, 2017 (post-outbreak)
- Volunteer hours: 431.5
- Schools affected by exclusion of non-immune students: 33
- Onset of first confirmed/probable case: Dec. 4, 2016
- Onset of last confirmed/probable case: June 5, 2017
- Highest number of cases reported in one week: 47
- Cases with complications:
- Orchitis: 2
- Oophoritis: 1
- Hearing loss: 1
- Mastitis: 1
- Meningitis: 1
- Encephalitis: 1
- Hospitalized: 1
- Calls taken by Washington Poison Center: 331
- MMR clinics held by local pharmacies: 31+
- Labor costs for four local pharmacies (Walgreens, Safeway, Albertson’s, and Rite Aid) to administer doses of MMR: $28,192
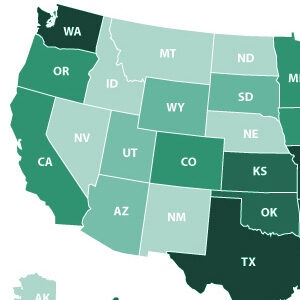
- Confirmed/probable cases in Washington State: 888
- Counties affected: 15
Behind the Scenes: Mumps Case Investigation
Many are unaware of the work that happens when a communicable disease is reported to the health district. While workload varies depending on the disease, investigations always have the same goal in mind—to prevent another case of the illness. Below is an example of a routine mumps investigation. A single mumps case investigation can take anywhere from two to six hours, depending on the complexity of the case.
- Report of child with parotitis received by SRHD.
- SRHD Epidemiology staff obtain medical records and, if necessary, coordinate laboratory testing.
- Epidemiology staff call the parents/guardians of the child to discuss the child’s symptoms and explore the source of the infection.
- Families are educated on infection control practices to use within their own home, as well as ensuring the ill child avoids contact with others until no longer contagious.
- Immunity status is verified for all family members and close contacts, and these individuals are educated on signs/symptoms of the disease and what to do if they develop.
- Child’s school nurse is notified prompting exposure notification to affected families.
- Epidemiology staff classify the case as confirmed, probable, suspect, or ruled out based on available information and DOH case classification rules.
- Staff report case to DOH.
Changes to Mumps Exclusion Recommendations
Under Washington law, health officers for local health jurisdictions are granted the authority to exclude susceptible, non-immune students from school settings as a control measure during disease outbreaks. Before and during the recent mumps outbreak in Washington State and Spokane County, DOH and SRHD officials recommended exclusion of non-immune students from schools with active mumps outbreaks for a full incubation period (up to 25 days) following their last exposure to a mumps case. During the 2016 - 2017 outbreak, 33 schools in four local districts were affected, including some for many weeks, as new cases continued to occur.
Thorough analysis of case data from the statewide outbreak provided DOH and health officers across the state the opportunity to examine all aspects of school exclusions for mumps cases and approve revised guidance. Beginning in September 2017, DOH officials updated recommendations that..."exclusion of non-immune students be considered," among the many means to control mumps outbreaks. Health officers are further encouraged to utilize exclusion in certain circumstances only, such as when severe illnesses occur beyond expected rates, when susceptible students are thought to be a major factor in disease transmission, etc. Reasons for the change in exclusion policy include:
- Rarity of mumps complications in the post-vaccine era.
- Scant numbers of unvaccinated students. Even though unvaccinated students are at greater risk for infection than vaccinated students, in most schools, they make up only a small proportion of the total student population, therefore the contribution of such unvaccinated students to transmission of mumps in recent outbreaks was relatively small.
- Relatively long incubation period of mumps. Exclusion of exposed students from school for two weeks or longer during ongoing outbreaks can significantly interfere with educational and extra-curricular activities resulting in hardship for students and families.
Recommendations from DOH and the Centers for Disease Control and Prevention (CDC) are particularly important for local health jurisdictions as they implement measures to prevent ongoing disease transmission. While SRHD staff remain hopeful that the community will be spared from another mumps outbreak, this revised guidance will assist in outbreak mitigation in the future.
